
Sergio Alejandro Alzate Cardozo1, Edgar Giovanny Ríos Dueñas MD2*, Msc (c), Juan Rafael Correa Ortiz MD3
1Cardiovascular Surgery at Pontificia Universidad Javeriana, Bogotá, Colombia
2Cardiovascular Surgeon at Hospital Universitario San Ignacio. Assistant Professor at Pontificia Universidad Javeriana School of Medicine, Bogotá, Colombia, Clinical Epidemiology Magister Candidate at PUJ
3Head of Cardiovascular Surgery, Cardiovascular Surgeon at Hospital Universitario San Ignacio, Bogotá, Colombia. Assistant Professor at Pontificia Universidad Javeriana School of Medicine.
*Corresponding Author: Edgar Giovanny Rios Dueñas, MD, Msc(c ). Cardiovascular Surgeon Hospital Universitario San Ignacio. Assistant Professor at Pontificia Universidad Javeriana School of Medicine, Bogotá, Colombia, Magister en Clinical Epidemiology Magister Candidate PUJ. Hospital San Ignacio, seventh floor, Cardiovascular Surgery Office.
Received date: March 02, 2022
Accepted date: March 07, 2022
Published date: March 11, 2022
Citation: Sergio Alejandro Alzate Cardozo, Edgar Giovanny Ríos Dueñas, Juan Rafael Correa Ortiz (2022) “Clinical and Post-Surgical Features and Outcomes in Post-Surgical Patients with Aortic arch Interruption at a Specialty Hospital in Bogotá Between 2006 and 2019.
Retrospective Multivariable Analysis.” International J of Clinical Cardiology and Cardiovascular Interventions, 2(4); DOI: http;//doi.org/04.2021/1.1010.
Copyright: © 2022 Edgar Giovanny Ríos Dueñas. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction. Interruption of the aortic arch due to absence of tissue between the ascending and descending portions of the aorta is a pathology of low incidence, yet it has a mortality rate of nearly 90% within the first year of life. Surgical intervention is aimed at re-establishing continuity of the vessel, as well as correcting associated lesions through closure of IVC or performing a pulmonary artery cerclage correction. The mortality is 18% to 42%. The survival rate is close to 73% at one month, 65% at one year and 63% at 3 years after surgery.
Materials and Methods. Review of Cardiovascular Surgery database between 2006 and 2019, identifying patients who underwent surgery due to aortic arch interruption.
Results. In the last 4 years, an institutional technique was introduced, using pericardium tissue for reconstruction and partial junction of the descending aorta with the arch through advancement of the arterial cannulae towards the brachiocephalic trunk and has been positively associated to brain protection. Since, results have improved: lower tissue traction, greater amplitude of the neoarch and better neurological outcomes have been achieved. The objective of this paper is to identify the most important factors that ultimately determine prognosis and survival of patients with these pathologies, as well as to describe results of the implemented technique.
Discussion. Aortic arch surgery is considered to be highly complex. Results yielded in this research showed a high mortality within the first years, which decreased into a similar rate to that of medical literature.
The main factors associated with complications identified were a late diagnosis and malnutrition. In addition, morbidity and mortality rates were similar to those reported worldwide.
Introduction
Interruption of aortic arch (IAA) is an infrequent congenital anomaly; its incidence is low (below 1%) and the mortality rate is close to 90% (in the prenatal period and the first year of life). It is featured by an absence of continuity (anatomic and luminal) of tissue between the ascending and descending aorta. It is frequently associated with other congenital malformations 1-3; there are reports in literature of patients with bicuspid aortic valve and other intra/extracardiac anomalies, such as right sided aortic arch, Fallot tetralogy malformation, ductus arteriosus, tricuspid atresia and great artery transposition. These associated anomalies have significant implications on the patients’ hemodynamic status, as well as the most suitable surgical strategy4.
The clinical presentation is characterized by cardiogenic shock or severe heart failure within the first two weeks of life 5, and approximately 50% of cases are documented in the context of DiGeorge Syndrome (microdeletion 22q11.2)6. Outflow tract hypoplasia is often found in cases of IAA, which complicates thesurgical approach 6. Fetal ultrasound allows for visualization of cardiac structures as of the second trimester of pregnancy, favoring early diagnosis of IAA and other anomalies 7. Recently, computer tomography has gained relevance as a reliable non-invasive diagnostic method for assessment of congenital cardiac diseases and great vessels with a sensitivity and specificity greater than 98% 4.
Depending on the location of the interruption of the arch, IAA is classified into 3 types 5,8. Type A IAA is characterized by an interruption located after the origin of the left subclavian artery, it is the second most common type of IAA and it is found in 30% to 40% of cases and it is associated mainly to hemodynamic factors related to blood flow 5. Type B IAA occurs due to an interruption between the site of origin of the common carotid and left subclavian arteries, it is the most common type of IAA, comprising 50% to 60% of cases and it is more closely related with DiGeorge Syndrome 5,7. Type C IAA is described as an interruption between the origin of the brachiocephalic trunk and the left common carotid artery, it is the least frequent type and is only found in 5% of cases 5.
Surgical reparation is the only viable treatment option and its goal is to re-establish continuity of the aortic arch and correct associated lesions. This is performed once hemodynamic stability is achieved after management with prostaglandin E1, thus avoiding closure of the ductus arteriosus 6. Since the first surgical reparation performed in 1955, several surgical techniques have been used. It remains a question under debate to determine which is the most suitable surgical technique for IAA reparation 9.
In the last 4 years, an institutional technique involving forward perfusion through the brachiocephalic trunk and widening of the aortic arch using an autologous pericardium patch was introduced. The goal of this paper is to identify the most important factors that determine prognosis and survival of patients with these pathologies and describe results of the use of this technique.
Methodology
In 2006, a Congenital Cardiopathy program started at the institution for this analysis with the aim of reducing mortality associated to complex, combined surgical procedures. Through its implementation, protocols have required modifications, learning curves and new techniques have been established with the aim of obtaining improved results. In the past 4 years, an institutional reconstruction technique was introduced, using extracorporeal circulation (ECC) and autologous pericardium tissue for reconstruction, as well as partial junctioning of the descending aorta with the arch at the posterior end and medial face; simultaneously protecting the brain and redirecting the EOPA arterial cannula towards the brachiocephalic trunk, then performing occlusion with a tourniquet tilted to 24 degrees, plus a widening of the aortic arch with a pericardium patch. This surgical technique showed better results due to the fact that less traction is generated and there is a greater resection of ductal tissue.
The data presented below was obtained retrospectively after reviewing the institution’s cardiovascular surgery database. Information was input according to the determined variables (demographics, signs and symptoms, methods diagnosis, surgical intervention and follow up ultrasound). Medical records of patients with inadequate registration of variables and those who could not be followed in the postoperative period were excluded. Finally, the data was compared to results from existing literature.
Results
Since the implementation of the Congenital Cardiopathy Program during the 2006 to 2019 period, 22 newborns were intervened due to complex aortic coarctation, hypoplastic aortic arch or interrupted aortic arch. All pregnancies had complete prenatal controls, with prenatal diagnosis achieved in 50% of cases. 59% of the patients were delivered via repeated C-section or due to fetal suffering. A diagnosis of preterm delivery before week 37 was documented in 22% and low weight for birth under 1500 grams in 27% of cases. A greater frequency was found in males (68%) compared to females (32%) with a ratio of 2:1. Prenatal diagnosis was confirmed via transthoracic ultrasound in 100% of cases and 18% of patients underwent angio-tomography guided reconstruction.
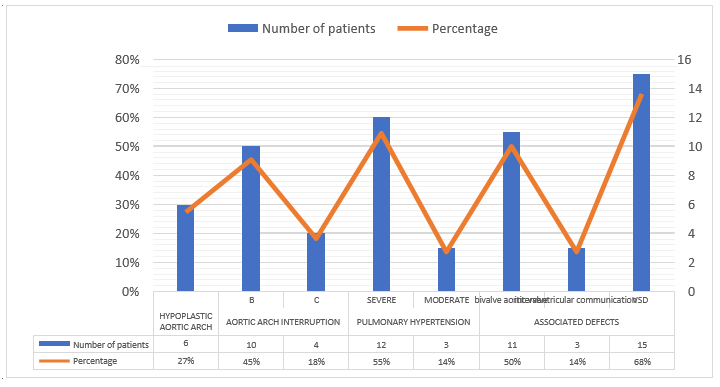
In Graph 1, most frequently associated pathologies, diagnosed by cardiac ultrasound. Other identified anomalies included great vessel transposition and ductus arteriosus in 4% and 4% of patients, respectively.
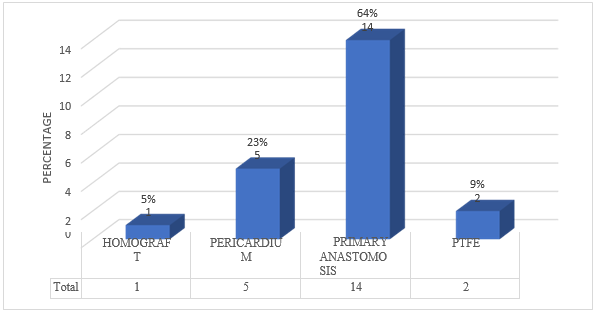
On average, patients underwent surgical correction on day 8 after birth, so that a weight of 3000 grams could be achieved (Graph 2). The main surgical procedure performed was primary anastomosis, in 50% of newborns. For the past four years, this technique was implemented with the widening technique using pericardium tissue (Graph 3). Other associated procedures are described in Graph 4.
Graph 2. Weight at.

Graph 3. Surgical procedure (primary: terminal-terminal anastomosis)
Graph 4. Associated surgeries (PDA: Persistent ductus arteriosus, IVC: interventricular communication, IAC interatrial communication)

Discussion
Surgical correction of IAA is a highly complex procedure and currently represents a challenge for cardiovascular surgeons because of its infrequent occurrence, which corresponds only to 1.5% of congenital cardiopathies and an incidence of 2 cases per every 100.000 live births 10.
A case series review of the period between 2006 and 2019 at a specialty hospital institution in the city of Bogotá. A documented 22 newborns underwent surgical procedures, the average age of the mother was 29 years, all pregnancies had complete prenatal controls, prenatal diagnosis was achieved in 50% of cases. A greater prevalence was documented for male newborns, corresponding to 68%; which is consistent with findings in literature reporting a 2:1 male to female ratio 12.
Diagnosis was confirmed afterwards by transthoracic cardiac ultrasound in 100% of patients, 18% of patients required angio-tomography reconstruction to more accurately define the anatomy. Type B IAA was documented in 55% of cases, followed by severe aortic arch hypoplasia in 27% of cases; type C IAA was reported in 18% of cases. These results are similar to those reported in literature, in which type B IAA is the most frequent at 50%, followed by type A in IAA at 30-40% and finally by type C at under 5% 11. Numbers of type A IAA were not reviewed in this case series due to the fact that these patients were managed as preductal aortic coarctation cases through a left thoracotomy approach and terminal-terminal anastomosis.
Associated cardiopathies are frequent in these cases, and include interventricular communication (68%), bivalve aortic valve (50%) and transposition of great vessels (4.5%). Intracardiac defects are reported in 95% of newborns with IAA (bivalve aorta and transposition of great vessels in lower proportion 12) as reported by statistical data on the behavior of this congenital malformation in Colombia.
Initial medical management is fundamental for treatment. Early treatment with prostaglandin E1 allows to maintain a permeable ductus arteriosus, improving distal perfusion distal and therefore improving the newborn’s condition, hemodynamic stabilization, compensation of heart failure and in addition weight gain is optimized. In this way, patients undergo the procedure with an average age of 8 days since birth, and an average weight of 3000 grams. In the last 4 years, newborns with types B and C IAA treated as severe hypoplasia of the aortic arch are corrected with ECC, using moderate hypothermia and forward perfusion through the brachiocephalic trunk, using an arch widening technique with autologous pericardium tissue in 89% of cases (8/9) and homologous graft (11%). This procedure reduced mortality, with a rate of 22% in contrast to 100% rate for techniques used previously, indicating a significant breakthrough for the management of this congenital malformation. In addition, cardiac ultrasound controls did not show significant gradients. The mortality rate of surgical reparation in a single intervention has been reported between 18- 42%.
The evidence reviewed shows that the described surgical technique benefits management of IAA patients given that a significant decrease in mortality that is consistent with international literature was observed. This data will serve as a foundation for future investigation in which determining factors for mortality and survival rates will be analyzed among patients treated for this congenital malformation in Colombia.
Conflict of Interest
The authors state they have no conflicts of interest.